Colorectal cancer, commonly known as colon cancer, is considered one of the leading cancer types worldwide. It develops in the large intestine (colon) or the rectum, and while it can be deadly if left untreated, it is also one of the most preventable types of cancer with proper awareness, lifestyle choices, and timely screening.
Many people are unaware that the digestive tract, from the mouth to the rectum, is nearly ten meters long if stretched out. The colon itself—around 1.5 meters in length—plays a vital role in processing waste and absorbing water from food. The inner lining of the colon is constantly renewing itself, which is normal. However, sometimes this process can go wrong, leading to the growth of extra cells in places where they shouldn’t be.
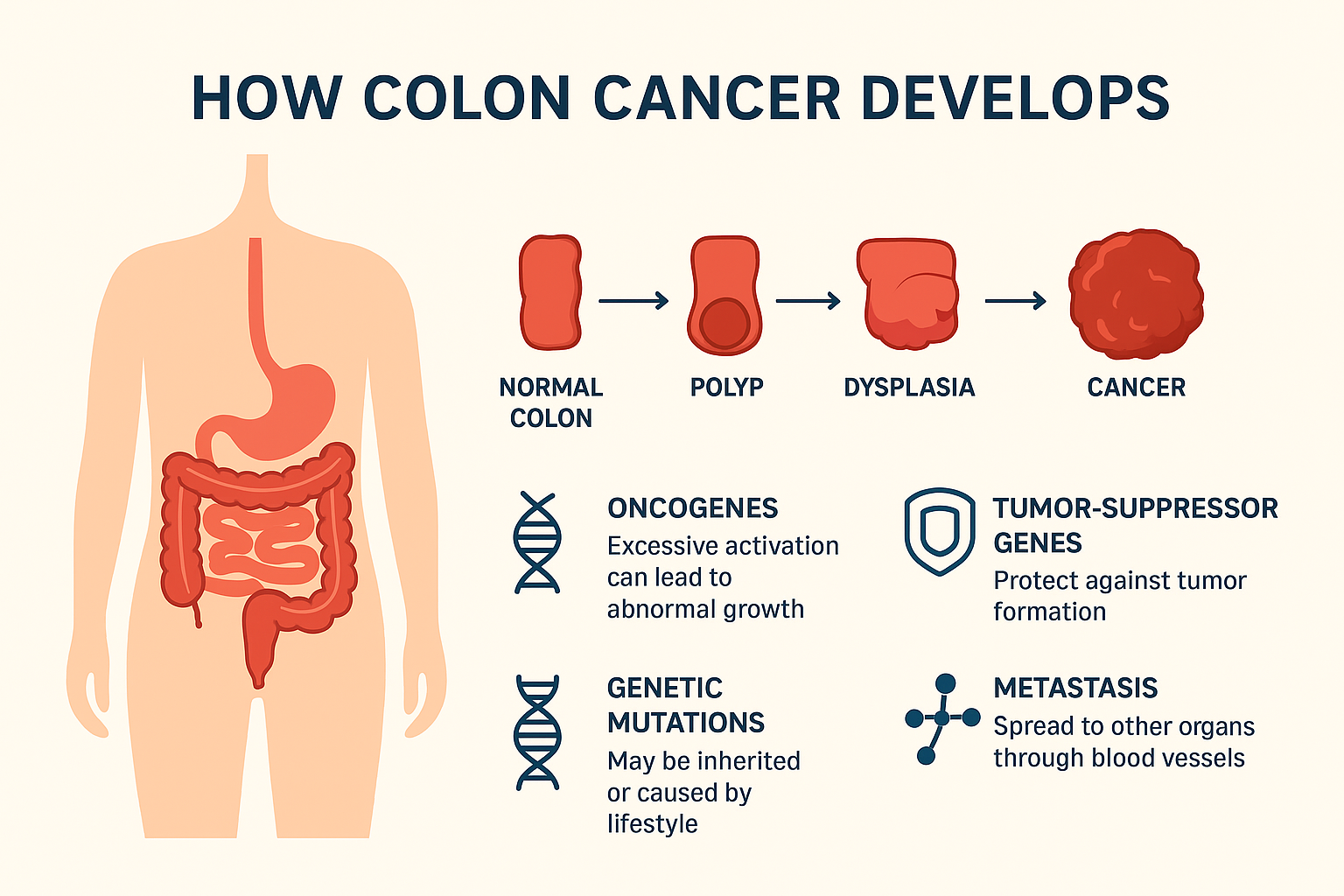
These unusual growths are called polyps. Most polyps are harmless, but some can turn into colon cancer over time if not detected and removed early. That’s why it is important for everyone to be aware of the causes, symptoms, and risk factors linked to colon cancer.

How Colon Cancer Develops
Colon cancer doesn’t appear suddenly. In fact, it can take 10 years or more for a small polyp to gradually turn into cancer. This slow progression gives us a critical advantage—if we detect and remove polyps early through regular screening, we can prevent the cancer from ever forming.
Researchers still don’t fully understand why some people develop polyps that turn cancerous, but science has identified some important contributing factors:
- Oncogenes are genetic elements which, if excessively activated, can stimulate abnormal cell growth and unchecked division.
- Tumor-suppressor genes serve as intrinsic regulators of cell growth. When their function is disrupted by mutations, it can lead to unchecked cell proliferation and the formation of tumors.
Genetic mutations may be inherited from your family or caused by environmental and lifestyle factors such as diet, smoking, alcohol use, and physical inactivity.
Once cancer cells break through the lining of the colon, they can spread (metastasize) to other parts of the body through blood or lymphatic vessels, making treatment more difficult.
Who’s at Risk for Colon Cancer?
Anyone can develop colon cancer, but certain groups of people have a higher risk:
1. Average Risk Group
- Individuals who are 50 years or older have a higher chance of developing colon cancer.
- However, recent studies show that cases are increasing in younger adults as well, which is why doctors are recommending earlier screenings.
2. High-Risk Group
- Family history – If you have a parent, sibling, or child who has had colon polyps or colon cancer, your risk is higher.
- Genetic syndromes – Conditions like Familial Adenomatous Polyposis (FAP) or Lynch syndrome significantly increase cancer risk.
- Inflammatory bowel diseases – Chronic conditions such as Crohn’s disease or ulcerative colitis can damage the colon over time.
- History of polyps – If you’ve had polyps before, you’re more likely to develop them again.
The ideal time to begin screening depends on your personal health and family history, so it’s important to consult your doctor for a plan that suits you best.
How Screening Works
Screening is the most effective way to prevent colon cancer because it can detect polyps before they become cancerous.
1. Colonoscopy
When it comes to detecting colon cancer, colonoscopy remains the gold standard and the most effective screening tool.
- A doctor inserts a thin, flexible tube with a camera into the colon.
- If polyps are found, they can be removed immediately through a procedure called polypectomy.
- Colonoscopy is generally recommended every 10 years for individuals with average risk, whereas those with higher risk factors may require shorter screening intervals.
2. Other Screening Methods
- Stool tests – Such tests are designed to identify traces of blood or genetic alterations in stool samples, which can serve as early indicators of colon cancer.
- CT colonography – A special imaging scan that provides a virtual view of the colon.
- Although flexible sigmoidoscopy resembles colonoscopy, it is restricted to evaluating just a portion of the colon rather than its complete length.
If cancer is detected, treatment may involve surgery, chemotherapy, or radiation therapy depending on the stage.
Early Warning Signs of Colon Cancer
One of the biggest challenges with colon cancer is that it often doesn’t show noticeable symptoms in the early stages. In most cases, the disease goes unnoticed until it has progressed significantly.
However, certain warning signs can help detect it sooner and potentially save your life.
1. Changes in Bowel Habits
If you notice sudden changes in your normal bathroom routine, such as:
- Persistent diarrhea
- Frequent constipation
- Narrow or ribbon-like stools
…this could be an indication of an obstruction affecting the colon.
2. Blood in Stool
This is regarded as one of the primary indicators associated with the condition.
- Bright red blood on the stool
- Black, tar-like stools (indicating hidden blood)
- While bleeding can sometimes be caused by hemorrhoids, you should never ignore it—especially if it’s persistent.
3. Persistent Abdominal Discomfort
Unexplained abdominal symptoms such as:
- Cramps
- Bloating
- Excessive gas
- General discomfort
…may suggest that your digestive system isn’t working properly.
4. Unexplained Weight Loss
If you’re losing weight without dieting or exercising, it could mean that cancer cells are consuming your body’s energy or that your digestive system isn’t absorbing nutrients properly.
5. Constant Fatigue
Feeling tired all the time—even after enough rest—may be due to anemia caused by internal bleeding in the colon.
6. Anemia (Iron Deficiency)
A sudden drop in iron levels without a clear cause could mean hidden blood loss from the colon, which is sometimes linked to colon cancer.
📌 Important: These symptoms are not always due to cancer, but if they persist, it’s essential to get a medical evaluation right away.
How to Lower Your Risk of Colon Cancer
You can’t change your genetics, but you can make lifestyle adjustments to significantly reduce your risk of colon cancer.
1. Eat a Healthy Diet
- Increase fiber intake – A healthy diet should emphasize the inclusion of whole grains, a variety of vegetables, fresh fruits, and legumes.
- Limit red and processed meats – Beef, pork, sausages, and processed meats are linked to higher colon cancer risk.
- Reduce sugar and high-fat foods – These contribute to obesity, which increases cancer risk.
2. Stay Physically Active
At least 30 minutes of moderate exercise daily—like walking, cycling, or swimming—can help maintain a healthy weight and improve colon health.
3. Maintain a Healthy Weight
Excess belly fat is linked to higher colon cancer risk, so aim for a healthy body mass index (BMI).
4. Avoid Smoking and Limit Alcohol
Both smoking and excessive alcohol use are linked to many cancers, including colon cancer.
5. Drink Plenty of Water
Staying hydrated supports digestion and helps keep the bowels moving smoothly.
6. Get Regular Screenings
- People over 50 should have a colonoscopy every 5–10 years.
- Individuals with a family history of colon cancer are advised to start screening earlier, typically around the age of 40, or as per their doctor’s guidance.
- For individuals with a history of polyp removal, consistent follow-up examinations are essential to reduce future risks.
Final Takeaway
Colon cancer prevention is very possible if you:
- Recognize the warning signs early
- Adopt a healthy lifestyle
- Stay consistent with screenings
Remember: The earlier colon cancer is detected, the higher the chances of successful treatment and complete recovery.
Why Prevention Matters
Colon cancer is considered one of the most preventable forms of cancer with proper screening and lifestyle measures. By removing polyps early and adopting a healthy lifestyle, you can reduce your risk by up to 70%. Unfortunately, many people delay screening due to fear, embarrassment, or lack of awareness—often with deadly consequences.
Key Takeaways
- Colon cancer often develops slowly, giving us time to detect and prevent it.
- Screening is strongly recommended for all individuals over the age of 50, and for younger people who carry certain risk factors.
- A healthy diet, regular exercise, and avoiding harmful habits can greatly reduce your chances.
- Early detection saves lives—don’t wait until symptoms appear.
Final Word: Colon cancer is common, but with knowledge, awareness, and proactive care, you can protect yourself and your loved ones from its dangers. Prevention truly is the best medicine.
If you don’t want to read, you can watch the video by clicking on this Link…
https://youtu.be/daqArpIXFcg?si=zXMjsxGab6kWa65G
Frequently Asked Questions
Q1. What is colorectal cancer and how does it develop?
A. Colorectal cancer begins in the large intestine (colon) or rectum, often from small growths called polyps. While most polyps are harmless, some can gradually turn into cancer over 10+ years if not detected and removed early.
Q2. Who is at risk of developing colon cancer?
A. Risk increases after age 50, but younger adults are also being diagnosed more often. Higher-risk groups include people with:
1. Family history of colon cancer or polyps
2. Genetic syndromes (FAP, Lynch syndrome)
3. Inflammatory bowel diseases (Crohn’s, ulcerative colitis)
4. A personal history of colon polyps
Q4. How can colon cancer be prevented?
A. You can lower your risk by:
1. Eating a high-fiber diet (whole grains, fruits, vegetables, legumes)
2. Limiting red and processed meats, sugar, and high-fat foods
3. Staying physically active (30 minutes daily)
4. Maintaining a healthy weight
5. Avoiding smoking and limiting alcohol
6. Drinking plenty of water
7. Getting regular screenings (colonoscopy every 5–10 years after 50, or earlier if at high risk)