What is Dengue Fever?
Dengue fever is a mosquito-borne viral illness that primarily spreads through the bite of infected female Aedes mosquitoes, especially Aedes aegypti and, to a lesser degree, Aedes albopictus. These mosquito species thrive in tropical and subtropical regions worldwide, making dengue a serious health challenge in parts of Asia, Latin America, and Africa. Belonging to the Flaviviridae family, the dengue virus causes the infection and appears in four connected serotypes: DENV-1, DENV-2, DENV-3, and DENV-4. Because of these variations, an individual can contract dengue up to four times during their life, each time from a different serotype. The illness can range from mild flu-like symptoms to severe, life-threatening conditions, including Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS).
How is Dengue Fever Transmitted?
Dengue fever is primarily transmitted through the bite of infected mosquitoes, specifically the Aedes aegypti and Aedes albopictus species. These mosquitoes are small, dark-colored, and can be identified by white markings on their legs and a marking in the shape of a lyre on the upper surface of their thorax. Unlike most mosquito species that typically feed at night, Aedes mosquitoes are daytime biters, showing peak activity in the early morning and late afternoon.
1. The Role of Aedes Mosquitoes
The main culprit behind dengue transmission is the Aedes aegypti mosquito, which thrives in urban and semi-urban environments. These mosquitoes prefer to breed in clean, stagnant water that is commonly found in and around human habitations. Common breeding grounds include flower pots, discarded tires, open water storage containers, buckets, and even bottle caps. Due to urbanization and improper waste disposal, these breeding sites are widely available, contributing to the increasing incidence of dengue in densely populated areas.
Aedes mosquitoes have a peculiar feeding habit—they take multiple short meals from different people in a single feeding period. This increases the chances of spreading the virus from an infected person to multiple individuals within a short span of time.
2. The Virus and Its Carrier
The dengue virus, which causes the disease, belongs to the Flavivirus genus and is classified into four different serotypes: DENV-1, DENV-2, DENV-3, and DENV-4. The virus is transmitted to the mosquito as it draws blood from an infected host. Inside the mosquito, the virus enters an extrinsic incubation phase of about 8 to 12 days, during which it multiplies and eventually reaches the mosquito’s salivary glands.
The presence of the virus in the salivary glands ensures the mosquito becomes a permanent source of infection. From that point on, every time the infected mosquito bites another human, it injects the virus through its saliva directly into the person’s bloodstream, starting a new cycle of infection.
3. Human-Mosquito-Human Transmission Cycle
The transmission cycle of dengue primarily involves humans and mosquitoes. The sequence is as follows:
- When feeding on someone with dengue, the mosquito picks up the virus and becomes a carrier.
- Within the mosquito’s body, the virus undergoes replication and eventually migrates to the salivary glands.
- The infected mosquito bites another healthy individual, passing the virus into their bloodstream.
- The new person develops the disease after an incubation period of 4–10 days.
Such a cycle greatly increases the chances of large-scale dengue outbreaks, especially in areas with heavy mosquito infestation and inadequate preventive actions.
4. Why Direct Human-to-Human Transmission Doesn’t Happen
Dengue virus does not spread through direct human contact, such as touching, hugging, or sharing food. It requires a mosquito as a carrier for transmission. On very rare occasions, dengue spreads through blood transfusion, organ transplant, or from mother to fetus during pregnancy, referred to as vertical transmission. These cases are uncommon compared to mosquito-borne transmission.
5. Factors That Increase Transmission Risk
Several environmental and social factors contribute to the spread of dengue:
- Urbanization and Population Growth: High population density provides more hosts for mosquitoes to feed on.
- Climate Conditions: Warm and humid climates favor mosquito breeding and virus replication.
- Water Storage Practices: Improperly stored water often serves as a breeding place for mosquitoes.
- Travel and Migration: People traveling from dengue-endemic areas can introduce the virus to new regions.
6. Preventing Dengue Transmission
Since the disease spreads through mosquitoes, controlling mosquito populations and preventing bites are the most effective measures. This includes:
- Eliminating stagnant water around homes.
- Using mosquito nets, window screens, and insect repellents.
- Wearing long-sleeved clothing to reduce skin exposure.
- Community-based fogging and spraying programs during outbreaks.
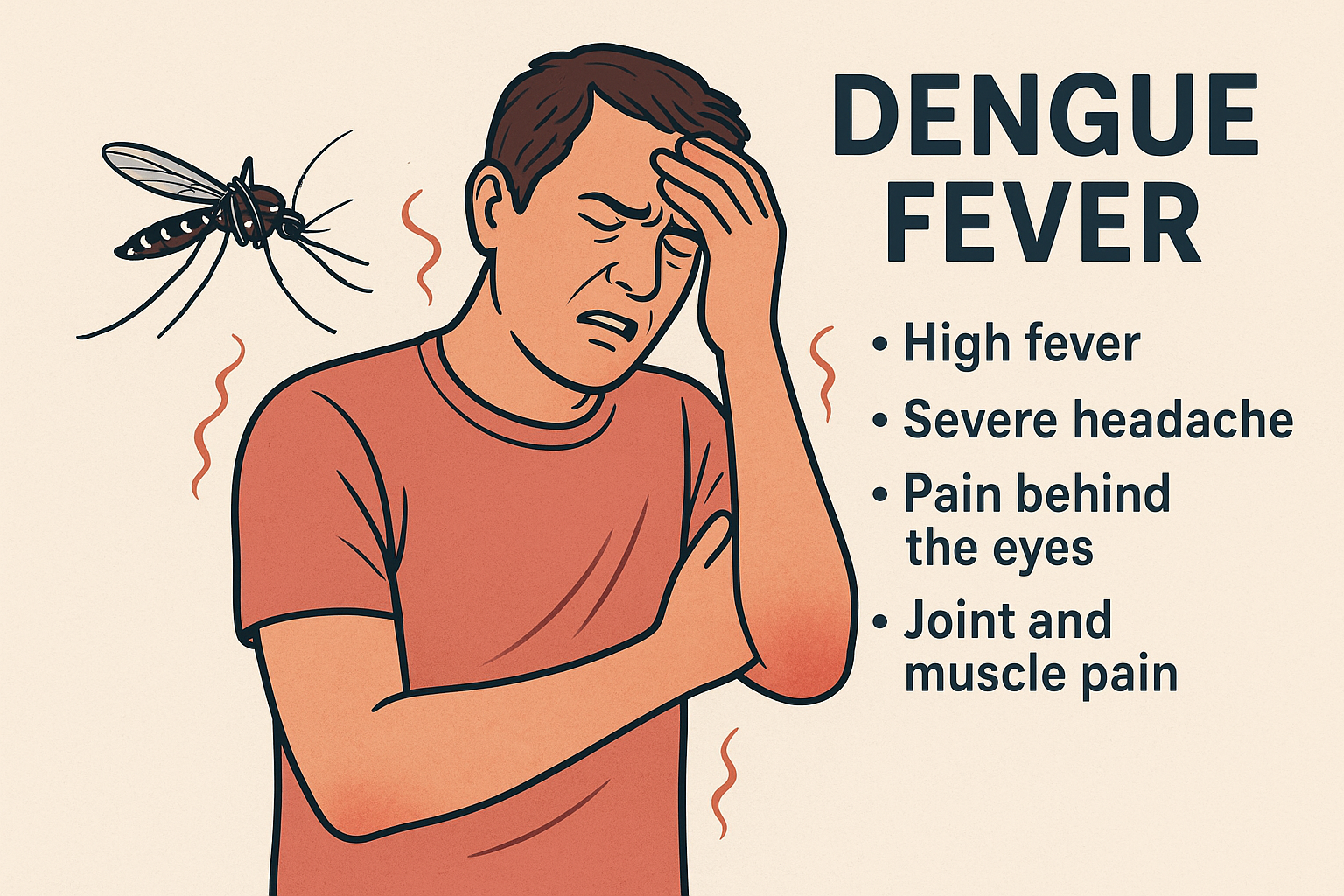
What Are the Symptoms of Dengue Fever?
Dengue fever symptoms can range from mild flu-like illness to severe life-threatening complications, depending on the stage and severity of infection. Understanding these symptoms is crucial because early detection and proper management can prevent the disease from progressing to dangerous stages like Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS). Below is a comprehensive, detailed explanation of the symptoms, their progression, and warning signs you should never ignore.
1. Incubation Period and Initial Signs
Following the bite of an infected Aedes mosquito, dengue virus enters the blood and begins its replication process. The incubation period, typically lasting 4 to 10 days, is when no symptoms are visible, yet the virus is rapidly multiplying within the body.
When the symptoms begin to appear, they often resemble common viral illnesses, which makes early detection challenging without proper medical testing. This is why many people initially confuse dengue with flu, chikungunya, or even COVID-19.
2. Common Symptoms of Dengue Fever
The early phase of dengue is usually identified by severe fever along with associated symptoms. Here are the most common signs in detail:
- High Fever (104°F or 40°C):
A rapid spike in body temperature is considered a classic symptom of dengue infection. The fever can last 2 to 7 days and may come in two phases (also called a saddleback fever pattern), where the temperature rises, drops, and rises again. - Severe Headache:
Intense pain, especially behind the eyes, is a distinctive symptom. This pain often worsens with eye movement. - Pain Behind the Eyes (Retro-Orbital Pain):
This is a unique feature of dengue, which helps differentiate it from common flu. - Joint and Muscle Pain:
The term “Breakbone Fever” is associated with dengue because of the severe muscle, joint, and bone pain that can make movement extremely difficult. - Nausea and Vomiting:
Digestive issues such as nausea, vomiting, and loss of appetite frequently accompany fever. - Skin Rash:
A red or pink rash often appears 2–5 days after fever begins. The rash may look similar to measles and usually starts on the chest before spreading to other body parts. - Mild Bleeding:
Some patients experience mild bleeding symptoms such as nosebleeds, gum bleeding, or easy bruising on the skin.
3. Progression to Severe Dengue (Warning Signs)
Most dengue cases are mild and recover without complications, but a few can progress to Severe Dengue, requiring urgent medical care. Warning signs often appear once the fever begins to subside and may include:
- Severe Abdominal Pain: Intense pain in the stomach area, which does not go away.
- Persistent Vomiting: Vomiting more than three times a day or inability to keep fluids down.
- Bleeding Symptoms: Nosebleeds, gum bleeding, blood in stool or vomit (black or tarry stools indicate internal bleeding).
- Rapid Breathing and Fatigue: Shortness of breath, extreme weakness, and restlessness.
- Enlarged Liver: Detected during medical examination.
- Drastic Drop in Platelet Count: A sudden fall in platelet levels increases the risk of internal bleeding and shock.
If any of these symptoms appear, hospitalization is necessary to prevent Dengue Shock Syndrome (DSS), where blood pressure drops dangerously low, leading to organ failure.
4. Phases of Dengue Symptoms
Dengue typically progresses in three phases:
- 1. Febrile Phase (2–7 days): This initial stage is marked by a sudden high fever, accompanied by severe headaches, muscle and joint aches, skin rashes, and nausea. Patients may feel weak and fatigued during this period as the body reacts to the infection.
- 2. Critical Phase (1–2 days after fever drops): Following the fever, some patients enter a critical window lasting about 24–48 hours. During this phase, plasma may leak from blood vessels, platelet counts can drop dangerously low, and there is a risk of bleeding and shock. Careful medical monitoring is essential to manage these complications.
- 3. Recovery Phase (2–3 days): In the recovery stage, symptoms gradually improve and vital signs stabilize. However, patients should continue to be observed closely to ensure there are no lingering complications or sudden relapses. Proper hydration, nutrition, and rest remain important for full recovery.
5. Why Symptoms Are Misleading
The challenge with dengue is that its early symptoms resemble flu, viral fever, or malaria, which leads to delayed diagnosis. This is why laboratory tests like NS1 antigen test, IgM/IgG antibody test, and complete blood count (CBC) are essential for confirmation.
✅ Summary of Symptoms
| Stage | Common Symptoms |
|---|---|
| Early (Febrile Phase) | High fever, headache, pain behind eyes, muscle & joint pain, nausea, rash |
| Warning Signs | Severe stomach pain, persistent vomiting, bleeding, rapid breathing, low platelets |
| Severe Dengue | Organ failure, severe bleeding, shock, death (if untreated) |
Why is Dengue Considered Dangerous?
Dengue fever is often misunderstood as a simple viral infection, but in reality, it has the potential to become life-threatening if not diagnosed and managed properly. While many cases of dengue are mild, some progress into severe stages that can lead to internal bleeding, organ failure, and even death. This is why dengue is considered one of the most dangerous mosquito-borne diseases in the world, affecting millions of people every year. Let us explore in detail why dengue is so dangerous.
1. High Rate of Infection and Rapid Spread
One of the primary reasons dengue is considered dangerous is its widespread nature and rapid transmission. According to the World Health Organization (WHO), about 390 million dengue infections occur annually, of which approximately 96 million manifest clinically. Endemic to over 100 countries, dengue primarily affects tropical and subtropical regions, putting about 50% of the global population in danger.
Unlike many other mosquito-borne diseases, dengue outbreaks occur in densely populated urban and semi-urban areas, where Aedes mosquitoes breed easily due to stagnant water and poor sanitation. The fast urbanization, increased travel, and climate change further contribute to its spread. The virus spreads rapidly during the rainy season, when mosquito breeding grounds are abundant, leading to sudden outbreaks and overwhelming local healthcare systems.
2. Absence of Specific Treatment or Cure
At present, dengue has no targeted antiviral therapy. Management primarily consists of maintaining adequate fluid balance, controlling high fever, and observing the patient for any warning symptoms that may indicate a severe form of the disease. Severe cases require hospitalization, intravenous fluids, and sometimes blood transfusions to manage bleeding and shock. Because there is no direct cure, the outcome depends largely on early detection and supportive care, which makes delayed diagnosis extremely risky.
3. Multiple Virus Serotypes and Risk of Reinfection
The dengue virus has four types—DENV-1, DENV-2, DENV-3, and DENV-4. Infection with one type ensures lifelong immunity only to that strain, leaving the person vulnerable to the others, which means dengue can strike up to four times.
What makes this even more dangerous is a phenomenon called Antibody-Dependent Enhancement (ADE). When someone who has previously had dengue gets infected with a different serotype, their immune system responds in a way that worsens the infection instead of fighting it. This increases the chances of developing Severe Dengue, making subsequent infections more dangerous than the first.
4. Severe Complications: Hemorrhage and Shock
Mild dengue symptoms, such as fever and body pain, usually resolve within a week. However, in some patients, especially during the critical phase (after the fever subsides), the disease can progress into Severe Dengue, which includes:
- Dengue Hemorrhagic Fever (DHF):
This condition is marked by bleeding from gums, nose, and under the skin, resulting in easy bruising. Patients may also experience internal bleeding, which is extremely dangerous and often goes unnoticed until it is too late. - Dengue Shock Syndrome (DSS):
This occurs when plasma leakage from blood vessels leads to a sudden drop in blood pressure, causing shock. DSS can rapidly lead to organ failure and death if not treated immediately. - Severe Organ Involvement:
In extreme cases, dengue can cause liver enlargement, heart complications, and neurological issues such as seizures or encephalitis.
5. Drastic Drop in Platelet Count
One of the most dangerous aspects of dengue is its effect on platelet count. Platelets are blood components responsible for clotting and preventing bleeding. A significant decline in platelet levels is common in dengue, which can lead to internal bleeding and potentially fatal hemorrhagic complications. A normal platelet count ranges from 150,000 to 450,000 per microliter, but in severe dengue, it can drop below 20,000, which is extremely dangerous.
6. Challenges in Diagnosis and Misinterpretation of Symptoms
Dengue symptoms—such as fever, headache, nausea, and body pain—are similar to many other illnesses like malaria, chikungunya, and viral flu. This makes early diagnosis difficult. Patients frequently dismiss early warning signs or rely on self-medication, resulting in delayed treatment and an increased risk of complications. By the time severe symptoms appear, the disease may have progressed to a critical stage, making hospitalization urgent.
7. High Mortality in Severe Cases
While the overall mortality rate for dengue is less than 1% with proper treatment, it can rise to 20% or more in severe cases without timely medical care. Children, pregnant women, and people with weak immunity are at higher risk of death from dengue complications.
8. Burden on Healthcare System
Healthcare facilities and hospitals experience immense strain during dengue outbreaks. During peak seasons, hospitals often run out of beds, blood supplies, and essential medicines. This lack of resources can lead to delays in treatment and higher fatality rates.
✅ Summary: Why is Dengue So Dangerous?
- No specific treatment or cure available.
- The disease spreads rapidly in cities, leading to a significant rise in infection rates.
- Four virus serotypes; risk of severe reinfection due to ADE.
- Severe complications like hemorrhage, shock, and organ failure.
- Drastic drop in platelet count increases risk of internal bleeding.
- Challenges in early diagnosis and treatment delays.
Prevention and Control Measures for Dengue Fever
Dengue fever is one of the fastest-growing mosquito-borne viral infections worldwide, and since there is no specific cure or widely available vaccine for all populations, the most effective way to Successful dengue prevention requires reducing mosquito populations and curbing their ability to transmit the disease. Dengue is primarily transmitted by the Aedes aegypti mosquito, and these mosquitoes thrive in urban and semi-urban environments where stagnant water is common. Understanding the strategies to prevent and control dengue is essential to reduce the risk of outbreaks and protect public health.
Here is an in-depth explanation of the methods used to prevent and manage the spread of the disease.
1. Source Reduction: Eliminating Mosquito Breeding Sites
The Aedes mosquitoes responsible for spreading dengue breed in stagnant, clean water, which is often found around homes, schools, offices, and construction sites. The first step in preventing dengue is removing these breeding habitats.
- Empty and Clean Water Containers:
Buckets, flower pots, bird baths, plant saucers, and pet water bowls should be emptied and cleaned at least once every week. - Proper Storage of Water:
If water must be stored, containers should be tightly covered to prevent mosquitoes from laying eggs. - Dispose of Waste Properly:
Discard unused tires, cans, and plastic containers that can collect water. These items are common mosquito breeding grounds. - Community Clean-Up Drives:
Community participation is essential. Neighborhood and public space cleanup initiatives, when properly organized, are highly effective in reducing potential breeding sites for mosquitoes.
2. Personal Protection Measures
Individual-level protection is equally important because mosquito bites are the main route of dengue transmission. Here are key personal preventive measures:
- Wear Protective Clothing:
Covering your body with long clothes and socks provides protection against mosquito bites. Mosquitoes are naturally drawn to darker colors, so wearing light-colored clothes can help reduce bites. - Use Mosquito Repellents:
Apply repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus on exposed skin. Reapply as recommended by the product label. - Use Mosquito Nets:
Sleeping under mosquito nets, especially during the day, is important because Aedes mosquitoes are daytime feeders. - Install Window and Door Screens:
Make sure doors and windows are fitted with mesh screens to block mosquitoes from coming inside.
3. Environmental Management
Creating an environment that is unfavorable for mosquito breeding is a long-term solution. This includes:
- Drainage Maintenance:
Clean clogged drains and gutters to avoid water stagnation. - Construction Site Monitoring:
Regular inspection of construction sites for standing water is essential, as these are high-risk areas. - Community Waste Management:
Proper garbage disposal and regular waste collection prevent accumulation of materials that can hold water.
4. Chemical Control Methods
In areas where dengue transmission is high, chemical interventions can be used to control mosquito populations:
- Larvicides:
Chemicals such as temephos can be added to water containers to kill mosquito larvae. These are safe when used in recommended doses. - Adulticides (Fogging):
Thermal fogging or ultra-low volume (ULV) spraying is often done during outbreaks to kill adult mosquitoes. It serves as a temporary fix and needs to be combined with efforts to eliminate breeding sources.
5. Biological Control Methods
Biological control is an eco-friendly approach to reducing mosquito populations:
- Larvivorous Fish:
Fish like Gambusia (mosquito fish) and guppy fish can be introduced into water bodies to feed on mosquito larvae. - Bacterial Control (Wolbachia Method):
Scientists are using Wolbachia-infected mosquitoes, which cannot transmit dengue virus. Releasing these mosquitoes in the environment has shown promising results in reducing dengue transmission in some countries.
6. Public Health Education and Awareness
Community awareness plays a critical role in dengue prevention. People should be educated about:
- The dangers of dengue and its symptoms.
- How mosquitoes breed and how to eliminate breeding sites.
- Importance of seeking early medical attention if symptoms appear.
Government campaigns, school programs, and social media outreach are effective ways to spread awareness.
7. Role of Government and Health Authorities
- Surveillance Programs:
Monitoring mosquito populations and disease incidence helps in early detection of outbreaks. - Integrated Vector Management (IVM):
A comprehensive approach combining chemical, biological, and environmental measures ensures long-term control. - Emergency Response Plans:
During dengue outbreaks, rapid action plans should be implemented, including fogging, hospital preparedness, and public announcements.
8. Vaccine and Research Efforts
Although prevention primarily depends on mosquito control, vaccines are also being developed. The Dengvaxia vaccine is available in some countries, but it is recommended only for individuals who have had a previous dengue infection. Scientists are working on newer, safer vaccines for broader use in the future.
✅ Summary of Key Prevention Steps
- Eliminate mosquito breeding sites (clean water storage, garbage disposal).
- Protect yourself with clothing, repellents, and mosquito nets.
- Use larvicides and fogging in high-risk areas.
- Promote community awareness and government-led campaigns.
Treatment Options for Dengue Fever
Dengue fever, caused by the dengue virus transmitted through Aedes mosquitoes, is a major public health concern worldwide. One of the biggest challenges in managing dengue is that there is no specific antiviral medication or universal cure available. Therefore, treatment primarily focuses on symptom relief, maintaining hydration, and preventing complications. The approach varies depending on whether the case is mild dengue or severe dengue (which includes Dengue Hemorrhagic Fever and Dengue Shock Syndrome). Below is a comprehensive, detailed explanation of treatment options for dengue fever.
1. General Principles of Dengue Treatment
- No Specific Antiviral:
Unlike bacterial infections that can be treated with antibiotics, dengue has no specific drug to kill the virus. - Supportive Care is Key:
The main goal is to manage fever, reduce pain, and maintain proper fluid balance to prevent dehydration and shock. - Early Diagnosis and Monitoring:
Timely medical attention significantly lowers the risk of severe complications. Medical professionals continuously monitor platelet count, hematocrit readings, and essential vital parameters during the course of the disease.
2. Outpatient Management for Mild Dengue
Most dengue cases are mild and do not require hospitalization. For such patients, home care under medical supervision is possible with the following measures:
a) Maintain Hydration
Fever, vomiting, and reduced appetite can lead to dehydration. To prevent this:
- Drink plenty of water, oral rehydration solutions (ORS), fruit juices, and soups.
- Coconut water is also recommended due to its natural electrolytes.
- Avoid caffeinated or sugary drinks.
b) Control Fever and Pain
- Use Paracetamol (Acetaminophen) to manage fever and pain.
- Avoid Aspirin, Ibuprofen, and other NSAIDs, as they increase the risk of bleeding by interfering with platelet function.
c) Rest and Nutrition
- Get adequate bed rest to support recovery.
- Consume light, easily digestible, nutritious food like soups, boiled vegetables, and fruits.
3. Hospitalization for Severe Dengue
Patients with warning signs or severe dengue require immediate hospitalization for intensive supportive care. Warning signs include:
- Persistent vomiting
- Severe abdominal pain
- Bleeding from gums or nose
- Black, tarry stools (sign of internal bleeding)
- Sudden drop in platelet count
- Restlessness or drowsiness
a) Intravenous (IV) Fluid Therapy
- IV fluids are administered to maintain proper hydration and prevent shock due to plasma leakage.
- The type and volume of fluids depend on the patient’s clinical status and hematocrit levels.
b) Blood and Platelet Transfusions
- In situations where platelet count falls under 20,000 and significant bleeding is present, doctors might recommend platelet transfusions.
- Whole blood or plasma transfusions may also be required for patients with heavy internal bleeding.
c) Oxygen Support and Monitoring
- Patients in Dengue Shock Syndrome need oxygen support and continuous monitoring of blood pressure, urine output, and vital signs.
4. Medications to Avoid in Dengue
- Aspirin, Ibuprofen, and NSAIDs: These drugs increase the risk of internal bleeding by affecting platelet function.
- Steroids: Not recommended because they do not improve outcomes and may cause harmful side effects.
5. Role of Alternative and Supportive Therapies
While there is no scientific evidence that herbal or alternative remedies cure dengue, some practices can complement medical treatment:
- Papaya Leaf Extract: Believed to help increase platelet count (research is limited and not conclusive).
- Giloy (Tinospora cordifolia): Used in traditional medicine for immunity boost, but should be taken only under professional advice.
Before attempting any home remedy, it is important to consult your doctor.
6. Prevention of Severe Complications
- Regular Monitoring: Daily platelet counts and hematocrit levels are critical.
- Refrain from taking medicines without medical advice, as incorrect drugs can have severe consequences in dengue.
- Early Hospitalization: If warning signs appear, immediate admission is essential to prevent progression to shock or organ failure.
7. Recovery and Post-Dengue Care
- Recovery usually takes 2–4 weeks after infection.
- Patients may experience fatigue, weakness, and hair loss during recovery.
- Proper nutrition, adequate hydration, and mild exercises are essential for restoring energy and overall recovery.
✅ Key Points to Remember
- No direct antiviral therapy is available for dengue at present, so management relies on symptomatic and supportive measures.
- Hydration and fever management are critical in mild cases.
- Hospitalization is required for severe dengue with complications like bleeding or shock.
- Avoid aspirin and NSAIDs because of bleeding risk.
- Early detection and timely medical intervention save lives.
If you don’t want to read, you can watch the video by clicking on this Link…
https://youtu.be/HAkYOOhbwos?si=shflZo-Y3SqXAKN-
https://youtu.be/6rn4DGcZQPw?si=Z-YdRmYXvtPt5Qz8
Frequently Asked Questions
Q1: What is dengue fever?
A: Dengue fever is a viral disease spread by Aedes mosquitoes. It can cause mild flu-like symptoms or severe conditions like Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS).
Q2: How is dengue fever transmitted?
A: Dengue spreads through the bite of infected Aedes mosquitoes (daytime biters). Direct human-to-human transmission is very rare, except in cases like blood transfusion or mother-to-child during pregnancy.
Q3: What are the common symptoms of dengue?
A:
1. High fever (up to 104°F / 40°C)
2. Severe headache and pain behind the eyes
3. Joint and muscle pain (“breakbone fever”)
4. Nausea and vomiting
5. Skin rash
6. Mild bleeding (nose, gums)1
Q4: What are the warning signs of severe dengue?
A:
1. Severe abdominal pain
2. Persistent vomiting
3. Bleeding (nose, gums, blood in stool or vomit)
4. Rapid breathing and extreme fatigue
5. Sudden drop in platelet count
6. Enlarged liver
Q5: Why is dengue considered dangerous?
A:
1. No specific antiviral treatment exists
2. Rapid spread in urban areas
3. Risk of severe reinfection due to 4 virus types
4. Can lead to complications like hemorrhage, shock, and organ failure
Q6: How can dengue be prevented?
A:
1. emove stagnant water where mosquitoes breed
2. Wear long clothes and use mosquito repellents
3. Sleep under mosquito nets and install window/door screens
4. Use larvicides and fogging in outbreak areas
5. Promote awareness and vaccination (if available)
Q7: How is dengue treated?
A:
1. Mild cases: Hydration, rest, paracetamol for fever/pain; avoid aspirin/NSAIDs
2. Severe cases: Hospitalization, IV fluids, blood or platelet transfusions, oxygen support, continuous monitoring
Q8: Can home remedies cure dengue?
A: No. Remedies like papaya leaf extract may support recovery but cannot cure dengue. Always consult a doctor.
Q9: How long is the incubation period?
A: Symptoms appear 4–10 days after the mosquito bite.
Q10: When should you see a doctor?
A:
1. If warning signs appear (vomiting, severe pain, bleeding, rapid breathing)
2. Symptoms last more than a week or worsen
3. Sudden drop in platelet count or suspected complications